Bone metastases, prostate cancer and theranostics
Bone metastases, prostate cancer and theranostics
Bone Metastases: A Common Secondary Cancer in Multiple Tumor Types
Bone metastases are a frequent complication in many cancer types, including breast (70%), prostate (85%), lung, and kidney cancers (40%), due to the unique characteristics of the bone microenvironment. Tumors predominantly metastasize to the axial skeleton—bones of the trunk and pelvis—rather than to the appendicular skeleton (limbs and girdles), following the distribution of red bone marrow.
Why Bone?
The bone is a highly vascular tissue that contains blood-forming stem cells and an active microenvironment that fosters cellular growth. While the process is not fully understood, the bone is rich in growth factors that cancer cells hijack and exploit for their own benefit. Healthy bone undergoes continuous remodeling, involving bone resorption (destruction) and new bone formation in a balanced cycle. This dynamic process also releases calcium, which is a critical component of bone turnover.
Cancer cells, which express calcium-sensing receptors, appear to take advantage of this constant supply of calcium, creating a fertile soil for tumor growth. Additionally, the unique immune environment in the bone, with both inhibitory and stimulatory effects on cells, may contribute to the proliferation of metastatic tumors. The slow blood flow within the red bone marrow also likely facilitates the attachment of cancer cells to the bone surface.
In osteoblastic metastasis (described below), studies have shown that cancer cells can mimic bone cells through "osteomimicry," by expressing bone-specific proteins. This allows them to evade immune detection, as the body mistakenly identifies them as healthy bone cells and "nurtures" rather than destroys them.
Metastatic Spread and Dormancy
Metastatic spread can begin early in the disease, even before the primary tumor is clinically detectable, and may remain dormant for years. The mechanisms that trigger these dormant cells to "wake up" and become active remain poorly understood and are the subject of ongoing research. Interactions between multiple cells in the bone microenvironment that maintain the dormancy and prevent its subsequent escape from quiescence are currently the target of clinical research.
Phenotypes of Bone Metastases
Bone metastases typically exhibit one of two phenotypes: osteoblastic (excessive bone formation) or osteolytic (bone destruction). Many metastases present a mixed phenotype, with one form predominating. Breast cancer often results in osteolytic bone metastases, while prostate cancer is known for its ability to stimulate abnormal bone formation, leading to osteoblastic metastases. Lung cancer bone metastases tend to be osteolytic.
Diagnostics of Bone Metastases
Bone metastases are often diagnosed at an advanced stage, with lesions already significant in size. Common symptoms include poorly localized bone pain, which worsens at night, pathological fractures, hypercalcemia (elevated calcium levels in the blood), and spinal cord compression. Blood tests may reveal anaemia, thrombocytopenia (low platelet count), or leukopenia (low white blood cell count). Timely and accurate diagnosis is crucial due to the significant clinical consequences of metastatic bone disease.
Standard-of-care imaging methods such as X-ray, CT scan, and radionuclide bone scintigraphy are routinely used to detect bone metastases, but these primarily reveal the body's response to cancer cells rather than directly visualizing the cancer itself. Biomarkers in blood and urine reflect overall bone resorption and formation but do not provide specific information about individual bone lesion sites.
Treatment Evaluation
Assessing the effects of treatment is equally important in clinical practice. Bone is the only metastatic site with distinct criteria for evaluating treatment response, which are based on the extent of bone repair and destruction rather than changes in tumor volume. Standard-of-care imaging techniques are often inadequate for treatment evaluation. A phenomenon known as the "flare response" may occur, where initial deterioration is detected in conventional imaging methods. This can lead to premature treatment discontinuation based on the false impression of ineffectiveness, when, in fact, the deterioration is followed by subsequent improvement.
Radioligand Lutetium-PSMA Therapy in Treating Metastatic Prostate Cancer
The detection of prostate-specific membrane antigen (PSMA) overexpression on prostate cancer cells has revolutionized the treatment of metastatic prostate cancer (mPC). Theranostics for mPC combines an imaging biomarker (PSMA-PET/CT using fluorine-18 or gallium-68) to detect and map tumor foci, regardless of their location, and predict treatment response. A radioligand, labelled with lutetium-177 or actinium-225, is then used to target and destroy the cancer cells directly. PSMA-PET/CT is also the most accurate tool available for treatment evaluation to date.
Read more about the diagnostics and therapy.
Therapy response example after 3 sessions of radioligand PSMA therapy with Lutetium-177 and 4-week intervals in-between
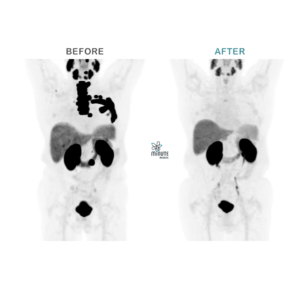
BEFORE
PSMA PET/CT January 2021
PSA 77 ng/ml
Metastasized castration resistant prostate cancer after several antihormonal treatments (1st & 2nd generation) and immunotherapy
AFTER
PSMA PET/CT December 2021
PSA 0,05 ng/ml
After 3x 177Lutetium PSMA ligand therapy January to March 2021 and no further therapy thereafter
Bibliography: Coleman, R.E., Croucher, P.I., Padhani, A.R. et al. Bone metastases. Nat Rev Dis Primers 6, 83 (2020). https://doi.org/10.1038/s41572-020-00216-3






