¹⁶¹Terbium-PSMA Radioligand Therapy in Prostate Cancer Brain Metastases
¹⁶¹Terbium-PSMA radioligand therapy in prostate cancer brain metastases
The following clinical case illustrates two important aspects of radioligand therapy in prostate cancer treatment. First, it is a highly effective approach capable of transforming the disease from potentially lethal to a manageable chronic condition, with occasional repeated cycles keeping it under control while preserving a good quality of life.
Second, Terbium-161 specifically can reach and treat challenging metastases, like those in the brain.
By the time Mr. G. arrived at our clinic in January 2021, his PSMA PET/CT showed widespread skeletal disease after a long and complex history of prior treatments.
He was first diagnosed with prostate cancer in January 2014 at 67 years old, after a blood test revealed an elevated PSA of 19 ng/ml. After robotic prostatectomy, radiation, and multiple lines of antihormonal and immunotherapy over the following six years, the disease continued to progress, with PSA rising steadily despite extensive pretreatment. By December 2020, after nearly every standard therapy had been tried, his PSA reached 60.7 ng/ml.
In early 2021, Mr. G. learned about radioligand therapy and decided to give it a go. He completed three sessions of 177Lu-PSMA between January and March 2021, achieving complete remission with undetectable PSA. Hormonal therapy was discontinued.
PSA began to rise again in late 2022, and by mid-2023 new bone lesions and a liver metastasis were detected, with PSA at 2.0 ng/ml in June 2023. Hormonal therapy was briefly restarted to upregulate PSMA (Lupron depot) before the next three-session cycle of radioligand therapy between August and October 2023. This cycle again resulted in complete remission, which lasted for 1.5 years.
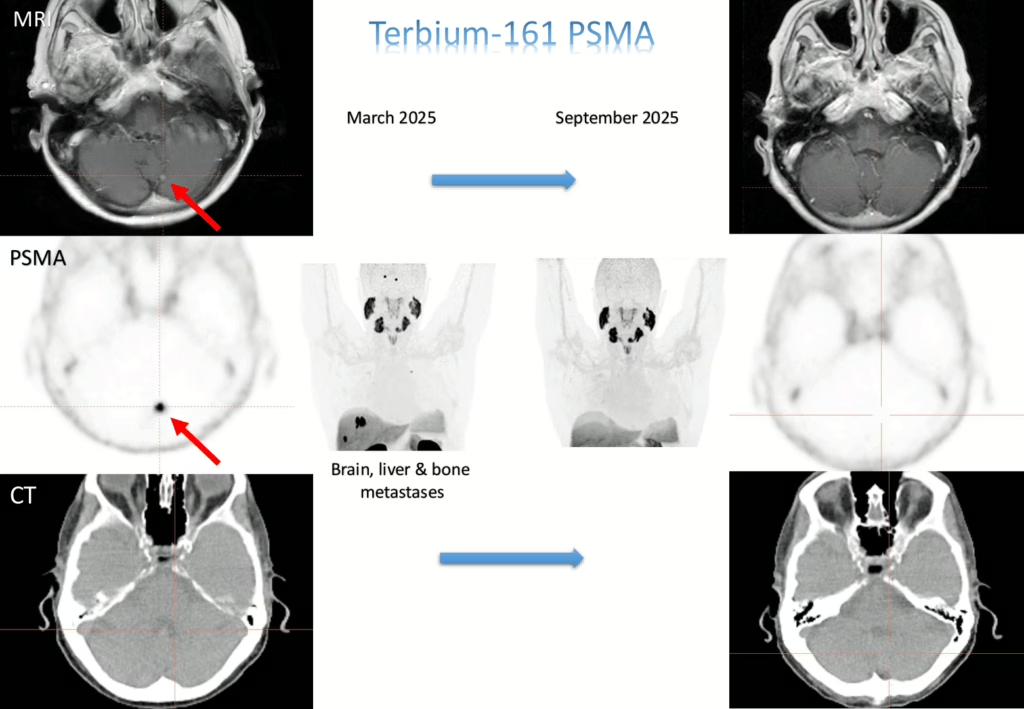
By March 2025, PSA had risen to 1.6 ng/ml, and PSMA PET/CT revealed new liver and cerebellar metastases. Given the complexity of the situation, the first two sessions were performed with the next-generation terbium-161 isotope, followed by a third session with the standard lutetium-177. This treatment led to a rapid PSA decline to 0.2 ng/ml, normalization of LDH (a general marker of disease activity), preserved kidney function, and only mild stable anemia. Throughout his treatment journey, Mr. G. has remained fully active, able to carry out all normal activities without restrictions, free of pain, and well-tolerant of therapy.
Follow-up PSMA PET/CT and brain MRI in September 2025 showed complete remission, with PSA once again undetectable.